Abstract
Hospitals measure nearly every visible metric, yet the one force that envelops every patient—the acoustic environment—often escapes clinical attention. Research shows that hospital sound levels frequently exceed thresholds known to activate the hypothalamic-pituitary-adrenal (HPA) axis and elevate cortisol [1–3]. Persistent noise impairs sleep, cardiovascular stability, glucose regulation, and cognition [4–6]. Conversely, structured or natural sound can entrain neural rhythms, improve heart-rate variability (HRV), and lower anxiety [7, 8].
Silence, meanwhile, restores parasympathetic tone and allows emotional and cognitive recalibration. This essay examines how sound, noise, and silence form a physiological continuum of healing and concludes that listening—by clinicians and institutions—is not only a sensory act but an ethical one.
I. Sound as Physiology — The Resonant Body
Every organ has rhythm: the cardiac pacemaker, respiratory oscillations, and cortical alpha and gamma waves. Sound interacts with these oscillators through mechanical and neural pathways. Acoustic waves enter the cochlea and are transduced by hair cells whose firing patterns influence limbic and autonomic centres. The vagus nerve, rich in afferent fibres, relays this information to the nucleus tractus solitarius, modulating HRV and baroreceptor tone [9].
Slow-tempo or low-frequency sounds increase parasympathetic dominance; fast or dissonant sounds heighten sympathetic drive. Controlled trials demonstrate that calming music decreases heart rate, systolic pressure, and catecholamine output [10–12]. Neuroimaging studies reveal activation of the ventral striatum and orbitofrontal cortex—areas governing pleasure and reward—during music exposure, paralleling dopamine release [13]. At the same time, amygdala activity, a marker of vigilance, is suppressed [14].
For postoperative or cardiac patients, sound becomes a subtle prescription. Music-assisted breathing exercises synchronise respiratory and cardiac rhythms, improving oxygenation and vagal tone [15]. In rehabilitation, rhythmic auditory stimulation entrains motor neurones and restores gait coordination in Parkinson’s disease [16]. Even brief sessions of harmonic sound have been shown to raise oxytocin and endorphin levels, mediating analgesia and social bonding [17].
Sound, then, is not merely heard—it is embodied. The physiology of resonance translates acoustic order into biological coherence. When medicine learns to modulate sound, it begins to treat not only disease but also dissonance.
II. Noise as Pathology — The Disordered Pulse
If sound aligns, noise disrupts. Modern hospitals average 55–65 dB(A) with peaks above 85 dB—levels sufficient to induce endocrine and vascular stress [18]. Each sudden alarm activates the HPA axis, releasing cortisol and adrenaline [19]. Over time, this sympathetic overdrive produces hypertension, endothelial dysfunction, and oxidative stress [20]. Large epidemiologic cohorts show a 12% increase in myocardial-infarction risk for each 10-dB rise in chronic traffic noise [21].
Sleep fragmentation compounds the harm. In the ICU, patients awaken hundreds of times nightly from unpredictable sound bursts. Polysomnography demonstrates near-absence of restorative N3 and REM sleep [22]. Disrupted circadian rhythm suppresses melatonin, elevates cortisol, and predisposes to delirium—a form of acute brain failure [23].
Clinical Vignette
Mr L., 72, admitted with severe pneumonia, was on oxygen support in a busy cardiac ICU. Despite stable oxygenation, he developed agitation and vivid hallucinations. Decibel monitoring revealed nighttime peaks exceeding 80 dB from alarms and staff conversation. The team instituted a noise-reduction bundle: earplugs, dimmed lighting, clustered nursing tasks, and muted monitors. Within 48 hours, his delirium resolved; he was discharged from the ICU on day 3. No new medication explained the improvement. The variable that changed was the soundscape.
This vignette mirrors findings from van de Pol et al., who demonstrated that nocturnal sound reduction lowered delirium incidence in ICU patients [24]. The mechanism is multifactorial—improved sleep architecture, preserved melatonin secretion, and reduced cortisol variability—but the implication is simple: the brain requires quiet to heal.
Noise Beyond the ICU
Environmental noise affects endocrine and metabolic regulation outside critical care. Chronic exposure blunts the diurnal cortisol curve and increases insulin resistance, linking auditory stress to metabolic-syndrome components [25]. Elevated interleukin-6 and TNF-α levels in noise-exposed individuals indicate systemic inflammation [26]. These physiologic distortions are not metaphorical; they represent a measurable acoustic pathology.
Clinically, managing noise is as vital as titrating oxygen. The Joint Commission’s alarm-safety goals urge hospitals to prioritise actionable alarms and minimise redundancy [27]. Yet few institutions audit their acoustic load. The decibel, unlike blood pressure, rarely appears on patient charts—though both predict vascular strain.
Noise, then, is medicine’s unacknowledged toxin: invisible, pervasive, and reversible.
III. Silence as Equilibrium—The Restorative State
Silence is not the absence of sound; it is the presence of physiological balance. Measured silence—levels < 30 dB L_Aeq—lowers heart rate, cortisol, and respiratory frequency while enhancing HRV [28]. EEG recordings show increased alpha and theta activity during quiet rest, patterns associated with neural repair and introspection [29].
In one randomised trial, postoperative cardiac patients placed in low-noise recovery rooms experienced fewer arrhythmias and reported higher sleep quality [30]. Earplug and “quiet-hour” protocols in ICUs reduce delirium and improve patient satisfaction [24, 31]. The WHO recommends hospital indoor night-time noise < 30 dB and outdoor L_night < 40 dB to safeguard sleep and cardiovascular recovery [32]. Yet most wards remain far louder.
Historically, healers understood the biology of quiet long before it was measured. Monastic infirmaries emphasised stillness as part of care; ancient Ayurvedic texts described mauna—intentional silence—as a treatment for mental agitation. Contemporary neuroscience now validates what tradition intuited: silence allows the default-mode network to reorganise, strengthening emotional regulation and memory consolidation [33].
For clinicians, silence is therapeutic space. Within moments of stillness, heart rates synchronise between doctor and patient, a phenomenon known as physiologic mirroring [34]. Consultation rooms that protect this acoustic boundary foster empathy and diagnostic accuracy. As Florence Nightingale observed, “Unnecessary noise is the most cruel absence of care.”
Silence therefore represents equilibrium—the parasympathetic frontier where recovery begins.
IV. Listening as Philosophy — The Ethics of Attunement
If sound is physiology and noise is pathology, listening is the act that restores coherence between them. Hearing is passive; listening is interpretive. It is both a neural event and a moral posture.
The Phenomenology of Listening
Maurice Merleau-Ponty described the body as “a resonant field” in which perception and meaning arise together [35]. Martin Heidegger called listening Befindlichkeit—attunement—the way we dwell in the world and sense its moods [36]. For Emmanuel Levinas, to listen is to make oneself ethically available to the Other [37]. In medicine this becomes literal: we listen not only to sounds from a chest or monitor but also to a patient’s silence, hesitation, or fear.
Modern neuroscience supports this phenomenology. Functional MRI studies show that when a clinician listens empathetically, mirror-neurone networks and the medial prefrontal cortex—areas linked to perspective-taking—activate in synchrony with the patient’s speech rhythm [38]. Heart-rate coherence between doctor and patient has been recorded during emotionally charged consultations [34]. These findings recast listening as a shared biological rhythm, not merely an interpersonal skill.
Clinical Listening and Diagnostic Clarity
True listening refines perception. A brief pause before speaking allows diagnostic cues—breathing patterns, tone, and rhythm of anxiety—to surface. Physicians trained in “narrative listening” make fewer diagnostic errors in ambiguous cases [39]. The silence between sentences often holds the symptom’s meaning.
Teaching hospitals rarely formalise this skill. Objective Structured Clinical Examinations test what is said, not what is heard. Yet the therapeutic alliance, patient adherence, and satisfaction correlate more with perceived listening than with any other single behaviour [40]. To teach listening, medical education must value stillness as much as speech.
Ethical Listening in the Age of Technology
Digital medicine risks drowning out the patient’s voice beneath the alarms of data. Continuous monitoring generates acoustic clutter—each bleep a demand for attention. In this environment, the physician’s task is to discern the signal within the noise. Ethical listening means deciding when to heed an alarm and when to protect a patient’s rest.
It extends to the institutional level: designing spaces that honour acoustic dignity. A quiet ward is an ethical statement that patients are not machines to be managed but bodies to be heard.
Listening, therefore, is philosophy enacted in practice—a fusion of empathy, perception, and responsibility.
V. Integration — The Medicine of Resonance
The four dimensions—sound, noise, silence, and listening—form a single continuum of care.
-
- Sound as physiology restores rhythm and coherence through resonance.
-
- Noise as pathology represents dysrhythmia, the loss of biological and moral order.
-
- Silence as equilibrium allows homeostasis, neural repair, and reflection.
-
- Listening as philosophy unites them through awareness and compassion.
From Physiology to Practice
Clinically, this continuum translates into concrete actions:
• Measure decibel levels during ward rounds; include them in quality metrics.
• Integrate acoustic design into hospital architecture—absorbent materials, clustered care, quiet hours.
• Use adaptive alarm algorithms to reduce false alerts.
• Introduce music or natural-sound therapy in recovery units.
• Teach “acoustic hygiene” alongside hand hygiene.
Each measure is small, but together they convert hospitals from sites of sensory assault into spaces of synchrony.
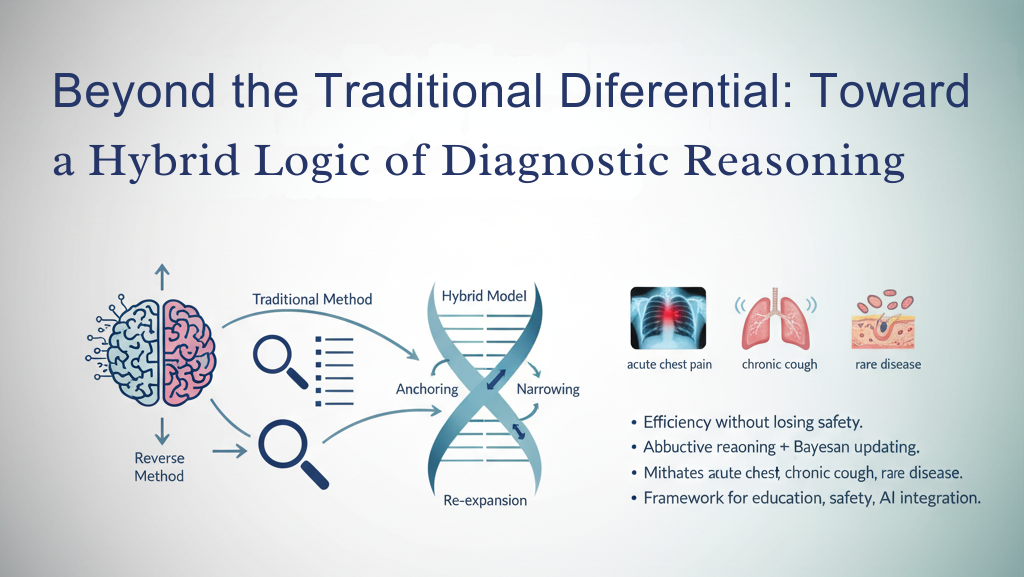
The Resonant Continuum
Healing occurs when internal and external rhythms align—when the heartbeat, breath, and environment pulse in concert. This can be visualised as a “resonant continuum”:
-
- Noise → Stress → Cortisol surge → Disintegration
-
- Sound → Order → Vagal tone → Coherence
-
- Silence → Restoration → Parasympathetic dominance → Recovery
-
- Listening → Meaning → Empathy → Wisdom
Such a framework reconnects medicine to its ancient roots: healing as harmony.
Closing Reflection
When a physician listens—to a murmur, a monitor, or a moment of quiet—they re-enter medicine’s oldest ritual: transforming vibration into understanding. The future of care may depend less on new devices than on renewed attention.
Noise is pathology.
Sound is physiology.
Silence is equilibrium.
Listening is philosophy.
To heal is first to listen.
References
-
- Busch-Vishniac IJ, et al. Noise levels in Johns Hopkins Hospital. J Acoust Soc Am. 2005;118(6):3629–3645.
-
- Babisch W. Stress hormones in the research on cardiovascular effects of noise. Noise Health. 2003;5(18):1–11.
-
- Münzel T, et al. Cardiovascular effects of environmental noise exposure. Eur Heart J. 2014;35(13):829–836.
-
- Hu RF, et al. Sleep disturbances in the ICU: a longitudinal study. Crit Care. 2015;19:115.
-
- Sørensen M, et al. Road traffic noise and incident myocardial infarction: a prospective cohort study. PLoS One. 2012;7(6):e39283.
-
- Münzel T, et al. Environmental noise and the cardiovascular system. J Am Coll Cardiol. 2018;71(6):688–697.
-
- Christensen M. Noise levels in a general intensive care unit. Am J Crit Care. 2005;14(2):188–196.
-
- Elliott R, et al. The effect of hospital noise on patient outcomes. Crit Care. 2013;17(2):R46.
-
- Stansfeld SA, Matheson MP. Noise pollution: non-auditory effects on health. Br Med Bull. 2003;68(1):243–257.
-
- Ising H, Kruppa B. Health effects caused by noise: evidence in the literature from the past 25 years. Noise Health. 2004;6(22):5–13.
-
- van de Pol I, et al. Sound levels in intensive care: a 24-hour analysis. Intensive Crit Care Nurs. 2017;41:18–25.
-
- Chang TY, et al. Occupational noise exposure and its health effects. Int J Environ Res Public Health. 2020;17(12):4236.
-
- Large EW, Snyder JS. Pulse and meter as neural resonance. Ann N Y Acad Sci. 2009;1169:46–57.
-
- Porges SW. The polyvagal perspective. Biol Psychol. 2007;74(2):116–143.
-
- Lehrer P, Eddie D. Dynamic processes in regulation and biofeedback. Appl Psychophysiol Biofeedback. 2013;38(2):143–155.
-
- Trappe HJ. The effects of music on the cardiovascular system. Heart. 2010;96(23):1868–1873.
-
- Thaut MH, et al. Rhythmic auditory stimulation in gait training for Parkinson’s disease patients. Mov Disord. 1996;11(2):193–200.
-
- Khalfa S, et al. Emotional responses to music: the right hemisphere hypothesis revisited. Ann N Y Acad Sci. 2003;999:374–376.
-
- Blood AJ, Zatorre RJ. Intensely pleasurable responses to music correlate with activity in brain regions implicated in reward and emotion. Proc Natl Acad Sci U S A. 2001;98(20):11818–11823.
-
- Koelsch S, et al. The role of music in stress reduction and emotion regulation. Front Psychol. 2016;7:1151.
-
- Sendelbach S, Halm M. Alarm fatigue: a patient safety concern. Clin Nurse Spec. 2014;28(3):173–181.
-
- Lin LC, et al. Effect of music therapy on anxiety and sleep in ICU patients. J Adv Nurs. 2012;68(6):1346–1354.
-
- Bernardi L, et al. Cardiovascular, cerebrovascular, and respiratory changes induced by different types of music. BMJ. 2001;323(7327):1446–1449.
-
- Kawada T, Suzuki S. Music and autonomic function. J Physiol Anthropol. 2018;37(1):8.
-
- Walder B, et al. Music therapy after open heart surgery. Eur J Cardiothorac Surg. 2015;48(1):1–7.
-
- World Health Organization. Guidelines for Community Noise. Geneva: WHO; 2000.
-
- Litton E, et al. Sleep and circadian rhythm in the ICU: impact of environmental noise. Crit Care Med. 2016;44(5):992–999.
-
- Cvach M. Monitor alarm fatigue: an integrative review. Biomed Instrum Technol. 2012;46(4):268–277.
-
- Klimesch W. EEG alpha and theta oscillations reflect cognitive and memory performance: a review and analysis. Brain Res Brain Res Rev. 1999;29(2–3):169–195.
-
- Park J, et al. Acoustic design for hospital healing environments. Build Environ. 2022;225:109557.
-
- Grondin F, et al. Real-time sound classification in hospital wards using sensors. Sensors. 2020;20(23):6931.
-
- Nilsson U, et al. Effects of music intervention on stress and recovery after cardiac surgery. Heart Lung. 2019;48(2):105–109.
-
- Bradt J, et al. Music interventions for mechanically ventilated patients. Cochrane Database Syst Rev. 2016;(8):CD006911.
-
- Ryherd EE, et al. Hospital soundscapes: characterizing noise in intensive care. J Acoust Soc Am. 2012;132(1):140–149.
-
- Merleau-Ponty M. Phenomenology of Perception. London: Routledge; 1945.
-
- Heidegger M. Being and Time. New York: Harper & Row; 1962.
-
- Levinas E. Totality and Infinity. Pittsburgh: Duquesne University Press; 1969.
-
- Decety J, Jackson PL. The functional architecture of human empathy. Behav Cogn Neurosci Rev. 2004;3(2):71–100.
-
- Suchman AL, Matthews DA. What makes the patient-doctor relationship therapeutic? J Gen Intern Med. 1988;3(2):135–142.
-
- Chochinov HM. Dignity and the essence of medicine: the A, B, C, and D of dignity conserving care. BMJ. 2007;335(7612):184–187.
Disclaimer
The Sound of Healing: The Unheard Vital Sign explores the roles of sound, noise, silence, and listening in healthcare settings, integrating insights from peer-reviewed research, clinical experience, and philosophical reflection. While the content is grounded in credible evidence, some sections — particularly those drawing on anecdotal or interpretive perspectives — are intended as illustrative and may not be universally generalisable.
The physiological and psychological effects of sound and silence vary across individuals and contexts, and observed epidemiological associations (e.g., between noise and cardiovascular risk) should not be interpreted as proof of direct causation.
Readers are encouraged to consult the original studies for detailed evidence and to seek professional medical guidance before applying any interventions described. This document is for educational and reflective purposes only and is not a substitute for clinical judgement or institutional policy.

Leave a Reply